Conference Program
View the SIG, RIG, and affinity group virtual meeting schedule.
Tuesday, April 5, 2022
11:00 am – 12 pm
Virtual Service & Outreach Event
Learn more about the SPPAC 2022 Service Projects & participate in a Sharing Circle/Women’s Empowerment Outreach Event with Achieving My Purpose (https://achievingmypurpose.org/). This activity is offered in collaboration with the Student/Trainee Antiracism Subgroup, Diversity SIG, & Student Advisory Board)
Contact: Juliana Yanguas, PsyD (jyangua1@jhmi.edu)
8:00 am
Registration and Check-In (ATRIUM)
10 am – 12:30 pm
Pre-conference Workshops
Addressing Structural and Institutional Barriers to Supporting Wellness for JEDI Warriors in Pediatric Psychology: A Trauma-Informed Call to Action
Amy Beck PhD - Children's Mercy Kansas City
Idia Thurston PhD - Texas A&M University
Christina Low Kapalu PhD - Children's Mercy Kansas City
Alexis Exum MPS MA - University of Kansas
Melissa Santos PhD - Connecticut Children's
Wendy Ward PhD ABPP FAPA FNAP - University of Arkansas for Medical Sciences
Lori Crosby PhD - Cincinnati Children's Hospital Medical Center
Pediatric psychologists exist within institutions where wellness is not always prioritized within the system; however, as psychologists, a key tenet of our training emphasizes wellness as an ethical imperative. When wellness is addressed within systems, it is infrequently tailored to the unique stressors/traumas that pediatric psychologists experience in the workplace. Equally overlooked are targeted wellness strategies for psychologists who experience racism at work, as well as psychologists who experience trauma from championing the dismantling of racist practices and systems. Pediatric psychologists are uniquely qualified to model innovative ways of embedding JEDI (Justice, Equity, Diversity, and Inclusion) principles into wellness strategies. Given that pediatric psychologists serve in diverse interdisciplinary and leadership roles, including clinical practice, training, research, and management, we are well positioned to advocate for these trauma-informed wellness strategies. To develop trauma-informed wellness programs that are tailored to persons of color and JEDI champions, it is important to identify the structural and institutional barriers to wellness that exist within systems and highlight the positive outcomes associated with removing these barriers(i.e., improving faculty and trainee wellbeing and retention, and improving patient outcomes). Further, institutional and personal wellness strategies are needed to promote the flourishing without re-traumatization of JEDI advocates. Our field is moving toward a more ethical, competent, and culturally humble practice, and thus it is necessary to advocate for the prioritization of trauma-informed wellness approaches at the institutional level. This process will create benefit for all institutional stakeholders. The proposed workshop will focus on increasing pediatric psychologists’ awareness of their own trauma related to racism and JEDI work, as well as support attendees in the creation of personalized wellness plans that increase capacity for thriving while disrupting and challenging barriers at the individual, interpersonal, and systemic levels. This workshop will focus on the following topics:
- Introduce a trauma-informed approach to wellness. (didactic)
- Identify the specific wellness needs of persons of color and JEDI advocates. (didactic)
- Facilitate a panel discussion with diverse (racial/ethnic; career development stages) pediatric psychologists regarding wellness in clinical practice, training, research, and management (panel discussion)
- Engage in a self-discovery activity with small groups (discussion and experiential)
- Create a personalized wellness plan (action)
- Practice mindfulness strategies tailored to JEDI work and advocacy (experiential)
This workshop is directly relevant to the conference theme given the focus on advocating for wellness, targeting strategies to enhance leadership, and promoting justice, equity, diversity and inclusion considerations.
Beyond Dysphoria: Adapting Interventions for Gender Diverse Youth
Kelsey MacDougall PsyD - MetroHealth Medical Center
Laura Edwards-Leeper PhD - Pacific University
Diane Chen PhD - Northwestern University Feinberg School of Medicine/ Ann & Robert H. Lurie Children’s Hospital of Chicago
Amy Tishelman PhD - Department of Psychology and Neuroscience Boston College
Claire Coyne PhD - Northwestern University Feinberg School of Medicine/ Ann & Robert H. Lurie Children’s Hospital of Chicago
Terry Stancin PhD - MetroHealth Medical Center/ Case Western Reserve University
Demand for gender affirming psychological services for youth has grown, including requests for psychotherapy (Chen et al. 2018). General medical and guidelines for clinical practice with transgender and gender nonconforming (TGNC) individuals are available, but there is limited evidence for psychological treatments, specifically interventions to support gender exploration and co-occurring conditions among TGNC youth. The purpose of this workshop is to fill a gap in existing practices by exploring and teaching specific problem focused interventions a pediatric psychologist may consider for a range of concerns commonly presented in gender diverse youth.The proposed structure of our workshop is to first broadly level set the audience with basic language and elements of guidelines for standards of care. Five national experts in gender diverse youth will then each discuss application of problem focused interventions followed by participant practice with interventions via small break out groups. The proposed topic areas include: Interventions in gender exploration in pre- and post-pubescent children/adolescents, applying the transgender resilience intervention model to TGNC youth with a stable gender identity, interventions and adaptations to trauma focused work, and practice in integrating various interventions into treatment planning for complex cases.Consistent with the theme of the conference, this workshop aims to advance practice and advocacy in the field of psychology by providing clinicians with the tools needed to serve a diverse group of protected individuals. An important aspect of work with TGNC youth is providing advocacy across systems including medical, school, family, and broader social settings.
Leading change: Using Quality Improvement to Bring Evidence-Based Approaches into the Pediatric Healthcare Setting
Amanda D. Deacy PhD - Children's Mercy Kansas City
Jennifer Schurman PhD - Children's Mercy Kansas City
Improving quality within complex health care systems can be deceptively challenging. In other words, what may seem like a simple “fix” often is not. While research helps us to understand what should work under ideal circumstances, quality improvement (QI) supports the process of uptake in real life clinical practice. Specifically, QI provides pediatric psychologists with flexible and powerful tools to become leaders in bringing evidence-based treatments into the practice setting and to advocate for consistent implementation of highest-quality health care on behalf of the patients and families we serve.Despite the clear benefits of QI methodology for closing the research-practice gap, few psychologists have had adequate training in QI methods to effectively lead a QI project. This workshop will provide a practical grounding in QI methods, from development of a QI charter with SMART performance goals articulated, through to hand-off to a process owner at project end for sustainability monitoring. Conceptual, practical, and regulatory considerations will be discussed. To illustrate these concepts, we will use our experience in implementing the Comfort Promise, an evidence-based bundled approach to minimizing pain with needle procedures, across our institution in a variety of settings and with a range of stakeholders. Specific project examples from this effort will be used to highlight key concepts in QI project development, execution, and write up. Specific to the goals of this year’s SPPAC, we will discuss the role of marketing and other advocacy efforts in supporting uptake of the Comfort Promise interventions across PDSA cycles, identify ways in which stakeholder voices, including those of patients and families, can be used to prioritize and drive local change, and highlight ways in which QI methodology can level the playing field and ensure equal access to care for all patients. We further will touch on the ethical implications of this type of work, including specifically shifting the institutional culture from provision of evidence-based care (i.e., pain prevention for needle procedures) being a nice thing to the right thing to do.Attendees with interest in either further developing their QI skills and/or in strategies for adopting evidence-based comfort measures as standard of care across needle procedures at their own institution will benefit from this workshop.
The Ethics of Power & Influence: Considerations for Medical Decision-Making & Advocacy
Mariella M. Self PhD ABPP - Baylor College of Medicine/Texas Children's Hospital
Debra Lefkowitz PsyD - Children's Hospital of Philadelphia
Pediatric psychologists often lead multi-faceted careers with opportunities to influence patients, families, colleagues, institutions or systems, science, and even society at large. The proposed workshop will focus on ethical considerations of power and influence in the various roles in which pediatric psychologists may function, addressing two specific topics: (1) choice architecture in medical decision-making and (2) the psychologist as advocate. Choice Architecture in Medical Decision-Making: Pediatric psychologists routinely work with patients and families navigating complex medical decision-making, frequently in a multidisciplinary context. Physicians and psychologists, either intentionally or unknowingly, can exert significant influence on treatment decisions through choice architecture, or the manner in which a choice is presented. This presentation will offer an overview of choice architecture and one of its prime concepts, nudging, with a focus on the attendant ethical considerations of its use in clinical practice. Specifically, nudging refers to strategic presentation of information or alternatives in a manner intended to alter behavior or steer health decisions. Types of nudges (e.g., framing, saliency, defaults, norms, messenger effects) will be illustrated, and evidence for their influence on medical decision-making will be reviewed. Ethical considerations in the strategic use of choice architecture will be addressed, and ethical claims made to justify or oppose nudging to shape decision-making (e.g., beneficence/best interest, autonomy/parental authority) will be discussed. Consideration will also be given to use of nudging in the context of culturally competent care. The Psychologist as Advocate: Pediatric psychologists can function as advocates at multiple levels, including advocating directly for a specific patient or advocating for policy at the institutional, local, state or federal levels. Likewise, psychologists’ skills in communication, relationship-building, strategic analysis and research can lend well to advocacy roles. This presentation examines different potential advocacy roles for psychologists, with consideration of the attendant ethical considerations, including patient confidentiality, conflicts of interest, conflicting values, and multiple relationships. Participants will also explore the question, “are psychologists ethically obligated to serve in advocacy roles?” Factors influencing the psychologist’s own personal and collective power will be examined, as well as the ways in which that power can be used for both positive and negative outcomes, particularly in advocating for marginalized populations.
1:30 pm – 2:30 pm
First-time Attendee Meet up
2:30 pm – 5 pm
Pre-conference Workshops
Anti-racism Efforts in Pediatric Psychology: Implementation of Training, Community, and Clinical Activism Efforts of the Anti-Racism Workgroup
Nicole Fleischer PsyD - St Christopher's Hospital for Children
Amy Hahn PhD - Nationwide Children's Hospital
Siddika Mulchan PsyD - Connecticut Children's
Caitlin Shneider MA - Georgia State University
Sobha Fritz PhD - Emory University School of Medicine
Elizabeth Getzoff Testa PhD - Mt Washington Pediatric Hospital
Monique Germone PhD - Children's Hospital Colorado
Claire Russell PhD - Bright Spark Therapy and Consulting
In response to extensive societal injustices, particularly the death of George Floyd at the hands of police officers, the Society of Pediatric Psychology recognized a need for more deliberate anti-racism work in our organization. As such, the Anti-racism Workgroup was formed in the summer of 2020 and several subgroups have committed to improving our organization through anti-racism efforts. Anti-racism work must be integral in all aspects of pediatric psychology, including research, advocacy, activism, and implementation, in order to address the impact of racism and systemic injustice on youth and families with whom we work. Given our ethical principles of Respect for People’s Rights and Dignity, Justice, and Beneficence and Nonmaleficence, psychologists are ethically responsible for anti-racism work. Therefore, the goal of this pre-conference workshop is to provide education, access to, and training of the anti-racism resources three subgroups (Training, Community, and Clinical) of the Workgroup have developed.First, the Training Subgroup will present the Diversity, Equity, and Inclusion in Supervision Self-Assessment Tool (DEI-SST) for clinical supervisors. Discussion topics will include: 1. The tool development process, 2. Proposed ways to utilize the DEI-SST, and 3. Review of other self-reflective tools to support a supervising psychologist’s antiracism journey as applied to clinical supervision.Second, the Community Subgroup will provide an overview of the current efforts to promote advocacy, policy change, community outreach, education, and promoting anti-racism within the pediatric psychology community. Presenters will introduce and discuss use of fact sheets on social determinants of health (SDoH), which were created to educate community health care providers, with the goal of targeting other systems affecting children's health (e.g., schools, law enforcement, etc.). Next, an overview of a program development project will be provided, which focused on a.) conducting a needs assessment among various community organizations devoted to children's needs, and b.) increasing exposure and education on a diverse workforce in pediatric psychology that will be shared with students in various levels of their education.Finally, the Clinical Subgroup will present clinical tip sheets, encompassing topics such as addressing implicit bias and talking about race with patients. Through use of role play, case vignettes, and discussion, participants will learn ways to implement anti-racism efforts into direct clinical work. Overall, this workshop will encourage and facilitate implementation of anti-racism efforts into several domains of pediatric psychology training, practice, and advocacy.
Developing a Peer Support Program within a Pediatric Healthcare System
Holly Antal PhD ABPP - Nemours Children's Health
Karen Wohlheiter PhD - Nemours Children's Health
Kathryn Godfrey PhD - ChristianaCare Hospital
Caroline Bruce RD LDN CDCES NASM-CPT - Nemours Children's Health
Peggy Greco PhD - Nemours Children's Health
Jennifer Shroff Pendley PhD - Nemours Children's Health
Loren Berman MD - Nemours Children's Health
Maureen Leffler DO MPH - Nemours Children's Health
Healthcare organizations are recognizing the importance of peer support programs in addressing provider burn-out, engagement, and well-being, particularly in the context of the significant and multifaceted stressors facing healthcare providers today. Acknowledging and providing support to colleagues has become more important than ever. While external resources of support (e.g, Employee Assistance Programs, EAP) are available, providers are inclined to talk to peers in stressful situations (Berman et al., 2021; Hu et al., 2012). Peer support programs offer free and confidential emotional support with nonjudgmental, active listening. Peer support can help provide support to all employees, both clinical and non-clinical, to help decrease workplace stress and burnout (Shapiro & McDonald, 2020). As pediatric psychologists focus on the care of children, their value in contributing to such programs may be initially overlooked. However, they are often the de-facto support system for pediatric medical colleagues and often provide support without a formal program. There are many benefits to establishing a formal program, including helping psychologists use their expertise to lead, train and support the work of peer support. The authors launched an enterprise-wide peer support program in May 2020 in consultation with the director of a well-established program at an affiliate hospital.This pre-conference workshop will 1) define peer support and describe programmatic implementation options; 2) provide attendees with peer support skills and resources to use within their own healthcare setting; 3) introduce pediatric psychologists to leadership opportunities that offer diversification of their traditional role in hospital settings, and 4) identify strategies for advocating with organizational leaders for both the implementation of a peer support program and for the role of psychologists in leading these efforts. This workshop will provide didactic instruction along with moderated breakout groups to facilitate role-play skills practice and feedback. Attendees will leave the session with skills and tools to initiate or expand a similar program of service within their own workplace setting. The content and goals of the proposed workshop align with the conference focus on broad leadership opportunities. The workshop includes specific strategies regarding how such a program addresses needs of underrepresented individuals who are experiencing stress relating to racial, gender, and other forms of micro- and macro-aggressions as well as oppression.
Promoting Health Equity with CLAS: Pediatric Psychology and the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care
Marilyn L. Sampilo PhD MPH - Cleveland Clinic Children's
Maxine Henry MSW MBA - National Latino Behavioral Health Association
Juliet Bui MPA MSW - U.S. Department of Health and Human Services Office of Minority Health
Advancing health equity means ensuring fair and just opportunities for all to attain optimal health. Unfortunately, structural inequities, including racism and discrimination, are deeply embedded within the system of healthcare manifesting as healthcare policy, procedures, and processes that contribute to a cycle of oppression and persistent behavioral health disparities (Gee & Ford, 2015). In order to move towards a more equitable society, structural inequities in healthcare must be addressed and these systems must move beyond diversity and inclusion to becoming intentionally equitable. Because pediatric psychology is uniquely positioned in its role at the intersection of youth, families, and the healthcare system, efforts must be undertaken to work towards a similar transformation. This means moving beyond the level of individual and interpersonal interactions to considering structural issues at broader levels (e.g. clinic/department/institution, community, policy) and developing structural competency (Metzl & Hansen, 2014). The National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care (National CLAS Standards; OMH, 2011) were developed to facilitate equitable and respectful care, thereby providing pediatric psychologists and their departments/agencies with a blueprint for promoting structural competency and implementing CLAS in pediatric psychology settings. Research suggests that after implementing CLAS, there are improvements in provider knowledge and skills, provider attitudes toward diverse patient populations, patient satisfaction, and patient-reported quality of care and trust in organizations (Weech-Maldonado et al., 2013).The proposed workshop will provide an overview of structural competency and the framework’s levels of interventions (Metzl & Hansen, 2014) as it relates to pediatric psychology, and will focus on CLAS as a mechanism to work towards structural competency as outlined by the National CLAS Standards. The workshop is intended to help attendees understand the role and application of structural and cultural competency to promote equity in pediatric psychology, and is intended to address the need for CLAS to improve care quality. The program is designed to 1) facilitate understanding of structural inequity and its manifestation in behavioral healthcare and pediatric psychology, 2) promote structural competency as a relevant framework for addressing disparities in pediatric psychology, 3) increase implementation of CLAS, including the National CLAS Standards, to increase capacity of pediatric psychology to promote equity, 4) provide practitioners and other key stakeholders with information that will help inform the development and implementation of equity strategies within their departments/agencies, and 5) position pediatric psychology professionals to lead equity initiatives at their home institutions.
School Advocacy for Children with Chronic Health Conditions: Opportunities for Pediatric Psychologists to Inform Stakeholders and Change Systems
Stephanie S. Filigno PhD - Cincinnati Children's Hospital Medical Center; University of Cincinnati College of Medicine
Amanda D. Deacy PhD BCB-A - Children’s Mercy Kansas City; University of Missouri Kansas City School of Medicine
Jennifer Lindwall PhD - University of Colorado; Children’s Hospital Colorado
Peter L. Stavinoha PhD ABPP - University of Texas MD Anderson Cancer Center & Children’s Cancer Hospital
Ginger Birnbaum BA
School engagement and success are important components of health-related quality of life for children with chronic medical conditions. Suboptimal school engagement can lead to academic underachievement and lower educational attainment, which can subsequently contribute to poorer quality of life in adulthood, including vocational achievement, relative to healthy peers. Even with clear evidence of significant educational risk related to chronic health conditions, research demonstrates that many, if not a majority, of youth with chronic conditions receive less academic support than they need and to which they are entitled.There is a critical need to attend to academic development of youth with chronic health issues more effectively and comprehensively. Fortunately, efforts are underway, in policy (e.g., Healthy People 2030), pediatrics, and education, to improve care coordination among relevant players in a chronically ill child’s community to support child and adolescent development in the academic arena. Key stakeholders include medical teams, allied health professionals, parents, educators, and administrators. Among these, pediatric psychologists are uniquely poised to contribute to these efforts, from early screening and in-depth assessment, to advocacy, guidance, innovative programming, and research. Additionally, pediatric psychologists are well-suited to consider barriers to educational advocacy unrelated to the medical condition, such as socioeconomic status and cultural and linguistic factors that may further complicate access to educational supports and services.This workshop will follow a practical, stepped-care model for advocating for the educational needs of youth with chronic health conditions. Specifically, the workshop will explore opportunities for pediatric psychologists to enhance advocacy for school engagement and success through both proactive assessment of educational risk and in-depth evaluation of cognitive and academic needs when appropriate. We will also discuss how to effectively participate in educational decision-making by refining the learner’s understanding of the eligibility process and identification of appropriate accommodations, problem-solve when school nomenclature and methodology for serving students is seemingly discordant with goals of clinical practice, and help stakeholders decode the language of both school and medical systems. An innovative hospital-based school program will be presented as an example of a “high-intensity” alternative academic setting for youth with complex medical, psychological, and social needs. As a final call to action, a parent provides a unique perspective to tie these concepts together and to represent the voice of patients and families.
So You Want to Start a Clinical Program? Best Practices and Considerations for Psychologists across Pediatric Healthcare Settings
Linda Herbert PhD - Children's National Hospital
Jessica Bernacki PhD - UCLA
Claire Ackerman PhD - Olentangy Pediatrics
Randi Streisand PhD - Children's National Hospital
The purpose of this workshop is to equip early career psychologists with skills and best practices for developing clinical programs across pediatric healthcare settings. Topics will include but are not limited to 1) assessing and addressing the needs of the patient population, including patients from frequently underserved populations, 2) working with multidisciplinary team members, 3) developing a business plan, 4) integrating trainees into the clinical program, 5) starting a clinical research program, and 6) adapting healthcare delivery to changing needs over time and making these program sustainable. The structure of this workshop is as follows:1) 1.5 hours of didactics from 4 presenters2) 1 hour of networking, during which attendees will have the opportunity to speak with 10 psychologists, from several sponsoring SIGs, who have started their own clinical programs or developed niche programs within existing clinical programs. This workshop is relevant to this year’s conference theme, Advancing Advocacy and Leadership through Science and Practice in Pediatric Psychology, in several ways. First, equipping early career psychologists with the skills they need to develop clinical programs empowers them to become leaders in their divisions, institutions, and the community. Further, the networking portion of this workshop will directly give attendees advice from psychologists who have “been there”. It will expand the network of psychologists that attendees can reach out to in the future for advice and assistance as they implement what they learned into their everyday work. We anticipate that participants will also be able to go back to their colleagues at their institutions and teach them about best practices for starting clinical programs. Second, this workshop will include best practices for developing clinical programs for patient populations who may not typically receive mental healthcare and advocating for additional support and is therefore relevant to the ‘advancing advocacy’ aspect of the conference theme.
Anti-racism Efforts in Pediatric Psychology: Implementation of Training, Community, and Clinical Activism Efforts of the Anti-Racism Workgroup
Nicole Fleischer PsyD - St Christopher's Hospital for Children
Amy Hahn PhD - Nationwide Children's Hospital
Siddika Mulchan PsyD - Connecticut Children's
Caitlin Shneider MA - Georgia State University
Sobha Fritz PhD - Emory University School of Medicine
Elizabeth Getzoff Testa PhD - Mt Washington Pediatric Hospital
Monique Germone PhD - Children's Hospital Colorado
Claire Russell PhD - Bright Spark Therapy and Consulting
In response to extensive societal injustices, particularly the death of George Floyd at the hands of police officers, the Society of Pediatric Psychology recognized a need for more deliberate anti-racism work in our organization. As such, the Anti-racism Workgroup was formed in the summer of 2020 and several subgroups have committed to improving our organization through anti-racism efforts. Anti-racism work must be integral in all aspects of pediatric psychology, including research, advocacy, activism, and implementation, in order to address the impact of racism and systemic injustice on youth and families with whom we work. Given our ethical principles of Respect for People’s Rights and Dignity, Justice, and Beneficence and Nonmaleficence, psychologists are ethically responsible for anti-racism work. Therefore, the goal of this pre-conference workshop is to provide education, access to, and training of the anti-racism resources three subgroups (Training, Community, and Clinical) of the Workgroup have developed.First, the Training Subgroup will present the Diversity, Equity, and Inclusion in Supervision Self-Assessment Tool (DEI-SST) for clinical supervisors. Discussion topics will include: 1. The tool development process, 2. Proposed ways to utilize the DEI-SST, and 3. Review of other self-reflective tools to support a supervising psychologist’s antiracism journey as applied to clinical supervision.Second, the Community Subgroup will provide an overview of the current efforts to promote advocacy, policy change, community outreach, education, and promoting anti-racism within the pediatric psychology community. Presenters will introduce and discuss use of fact sheets on social determinants of health (SDoH), which were created to educate community health care providers, with the goal of targeting other systems affecting children's health (e.g., schools, law enforcement, etc.). Next, an overview of a program development project will be provided, which focused on a.) conducting a needs assessment among various community organizations devoted to children's needs, and b.) increasing exposure and education on a diverse workforce in pediatric psychology that will be shared with students in various levels of their education.Finally, the Clinical Subgroup will present clinical tip sheets, encompassing topics such as addressing implicit bias and talking about race with patients. Through use of role play, case vignettes, and discussion, participants will learn ways to implement anti-racism efforts into direct clinical work. Overall, this workshop will encourage and facilitate implementation of anti-racism efforts into several domains of pediatric psychology training, practice, and advocacy.
Developing a Peer Support Program within a Pediatric Healthcare System
Holly Antal PhD ABPP - Nemours Children's Health
Karen Wohlheiter PhD - Nemours Children's Health
Kathryn Godfrey PhD - ChristianaCare Hospital
Caroline Bruce RD LDN CDCES NASM-CPT - Nemours Children's Health
Peggy Greco PhD - Nemours Children's Health
Jennifer Shroff Pendley PhD - Nemours Children's Health
Loren Berman MD - Nemours Children's Health
Maureen Leffler DO MPH - Nemours Children's Health
Healthcare organizations are recognizing the importance of peer support programs in addressing provider burn-out, engagement, and well-being, particularly in the context of the significant and multifaceted stressors facing healthcare providers today. Acknowledging and providing support to colleagues has become more important than ever. While external resources of support (e.g, Employee Assistance Programs, EAP) are available, providers are inclined to talk to peers in stressful situations (Berman et al., 2021; Hu et al., 2012). Peer support programs offer free and confidential emotional support with nonjudgmental, active listening. Peer support can help provide support to all employees, both clinical and non-clinical, to help decrease workplace stress and burnout (Shapiro & McDonald, 2020). As pediatric psychologists focus on the care of children, their value in contributing to such programs may be initially overlooked. However, they are often the de-facto support system for pediatric medical colleagues and often provide support without a formal program. There are many benefits to establishing a formal program, including helping psychologists use their expertise to lead, train and support the work of peer support. The authors launched an enterprise-wide peer support program in May 2020 in consultation with the director of a well-established program at an affiliate hospital.This pre-conference workshop will 1) define peer support and describe programmatic implementation options; 2) provide attendees with peer support skills and resources to use within their own healthcare setting; 3) introduce pediatric psychologists to leadership opportunities that offer diversification of their traditional role in hospital settings, and 4) identify strategies for advocating with organizational leaders for both the implementation of a peer support program and for the role of psychologists in leading these efforts. This workshop will provide didactic instruction along with moderated breakout groups to facilitate role-play skills practice and feedback. Attendees will leave the session with skills and tools to initiate or expand a similar program of service within their own workplace setting. The content and goals of the proposed workshop align with the conference focus on broad leadership opportunities. The workshop includes specific strategies regarding how such a program addresses needs of underrepresented individuals who are experiencing stress relating to racial, gender, and other forms of micro- and macro-aggressions as well as oppression.
Promoting Health Equity with CLAS: Pediatric Psychology and the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care
Marilyn L. Sampilo PhD MPH - Cleveland Clinic Children's
Maxine Henry MSW MBA - National Latino Behavioral Health Association
Juliet Bui MPA MSW - U.S. Department of Health and Human Services Office of Minority Health
Advancing health equity means ensuring fair and just opportunities for all to attain optimal health. Unfortunately, structural inequities, including racism and discrimination, are deeply embedded within the system of healthcare manifesting as healthcare policy, procedures, and processes that contribute to a cycle of oppression and persistent behavioral health disparities (Gee & Ford, 2015). In order to move towards a more equitable society, structural inequities in healthcare must be addressed and these systems must move beyond diversity and inclusion to becoming intentionally equitable. Because pediatric psychology is uniquely positioned in its role at the intersection of youth, families, and the healthcare system, efforts must be undertaken to work towards a similar transformation. This means moving beyond the level of individual and interpersonal interactions to considering structural issues at broader levels (e.g. clinic/department/institution, community, policy) and developing structural competency (Metzl & Hansen, 2014). The National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care (National CLAS Standards; OMH, 2011) were developed to facilitate equitable and respectful care, thereby providing pediatric psychologists and their departments/agencies with a blueprint for promoting structural competency and implementing CLAS in pediatric psychology settings. Research suggests that after implementing CLAS, there are improvements in provider knowledge and skills, provider attitudes toward diverse patient populations, patient satisfaction, and patient-reported quality of care and trust in organizations (Weech-Maldonado et al., 2013).The proposed workshop will provide an overview of structural competency and the framework’s levels of interventions (Metzl & Hansen, 2014) as it relates to pediatric psychology, and will focus on CLAS as a mechanism to work towards structural competency as outlined by the National CLAS Standards. The workshop is intended to help attendees understand the role and application of structural and cultural competency to promote equity in pediatric psychology, and is intended to address the need for CLAS to improve care quality. The program is designed to 1) facilitate understanding of structural inequity and its manifestation in behavioral healthcare and pediatric psychology, 2) promote structural competency as a relevant framework for addressing disparities in pediatric psychology, 3) increase implementation of CLAS, including the National CLAS Standards, to increase capacity of pediatric psychology to promote equity, 4) provide practitioners and other key stakeholders with information that will help inform the development and implementation of equity strategies within their departments/agencies, and 5) position pediatric psychology professionals to lead equity initiatives at their home institutions.
School Advocacy for Children with Chronic Health Conditions: Opportunities for Pediatric Psychologists to Inform Stakeholders and Change Systems
Stephanie S. Filigno PhD - Cincinnati Children's Hospital Medical Center; University of Cincinnati College of Medicine
Amanda D. Deacy PhD BCB-A - Children’s Mercy Kansas City; University of Missouri Kansas City School of Medicine
Jennifer Lindwall PhD - University of Colorado; Children’s Hospital Colorado
Peter L. Stavinoha PhD ABPP - University of Texas MD Anderson Cancer Center & Children’s Cancer Hospital
Ginger Birnbaum BA
School engagement and success are important components of health-related quality of life for children with chronic medical conditions. Suboptimal school engagement can lead to academic underachievement and lower educational attainment, which can subsequently contribute to poorer quality of life in adulthood, including vocational achievement, relative to healthy peers. Even with clear evidence of significant educational risk related to chronic health conditions, research demonstrates that many, if not a majority, of youth with chronic conditions receive less academic support than they need and to which they are entitled.There is a critical need to attend to academic development of youth with chronic health issues more effectively and comprehensively. Fortunately, efforts are underway, in policy (e.g., Healthy People 2030), pediatrics, and education, to improve care coordination among relevant players in a chronically ill child’s community to support child and adolescent development in the academic arena. Key stakeholders include medical teams, allied health professionals, parents, educators, and administrators. Among these, pediatric psychologists are uniquely poised to contribute to these efforts, from early screening and in-depth assessment, to advocacy, guidance, innovative programming, and research. Additionally, pediatric psychologists are well-suited to consider barriers to educational advocacy unrelated to the medical condition, such as socioeconomic status and cultural and linguistic factors that may further complicate access to educational supports and services.This workshop will follow a practical, stepped-care model for advocating for the educational needs of youth with chronic health conditions. Specifically, the workshop will explore opportunities for pediatric psychologists to enhance advocacy for school engagement and success through both proactive assessment of educational risk and in-depth evaluation of cognitive and academic needs when appropriate. We will also discuss how to effectively participate in educational decision-making by refining the learner’s understanding of the eligibility process and identification of appropriate accommodations, problem-solve when school nomenclature and methodology for serving students is seemingly discordant with goals of clinical practice, and help stakeholders decode the language of both school and medical systems. An innovative hospital-based school program will be presented as an example of a “high-intensity” alternative academic setting for youth with complex medical, psychological, and social needs. As a final call to action, a parent provides a unique perspective to tie these concepts together and to represent the voice of patients and families.
So You Want to Start a Clinical Program? Best Practices and Considerations for Psychologists across Pediatric Healthcare Settings
Linda Herbert PhD - Children's National Hospital
Jessica Bernacki PhD - UCLA
Claire Ackerman PhD - Olentangy Pediatrics
Randi Streisand PhD - Children's National Hospital
The purpose of this workshop is to equip early career psychologists with skills and best practices for developing clinical programs across pediatric healthcare settings. Topics will include but are not limited to 1) assessing and addressing the needs of the patient population, including patients from frequently underserved populations, 2) working with multidisciplinary team members, 3) developing a business plan, 4) integrating trainees into the clinical program, 5) starting a clinical research program, and 6) adapting healthcare delivery to changing needs over time and making these program sustainable. The structure of this workshop is as follows:1) 1.5 hours of didactics from 4 presenters2) 1 hour of networking, during which attendees will have the opportunity to speak with 10 psychologists, from several sponsoring SIGs, who have started their own clinical programs or developed niche programs within existing clinical programs. This workshop is relevant to this year’s conference theme, Advancing Advocacy and Leadership through Science and Practice in Pediatric Psychology, in several ways. First, equipping early career psychologists with the skills they need to develop clinical programs empowers them to become leaders in their divisions, institutions, and the community. Further, the networking portion of this workshop will directly give attendees advice from psychologists who have “been there”. It will expand the network of psychologists that attendees can reach out to in the future for advice and assistance as they implement what they learned into their everyday work. We anticipate that participants will also be able to go back to their colleagues at their institutions and teach them about best practices for starting clinical programs. Second, this workshop will include best practices for developing clinical programs for patient populations who may not typically receive mental healthcare and advocating for additional support and is therefore relevant to the ‘advancing advocacy’ aspect of the conference theme.
3:30 pm - 6:30 pm
Off-Site Service & Outreach Event at The Society of St. Vincent de Paul
Location: 2120 South 3rd Street, Phoenix, AZ 85003
Advanced Sign-Up and Masks Required
Join us for an afternoon of service at the Society of St. Vincent de Paul (a short walk from the conference hotel). Activities include assisting with meal service for families and providing after-school support for children.
This activity is offered in collaboration with the Student/Trainee Antiracism Subgroup, Diversity SIG, and Student Advisory Board.
Contact: Desireé Williford, PhD, MPH (desiree.williford@cchmc.org) and Rachel Fisher, MS (Rachel.Fisher10@okstate.edu)
4:00 pm - 5:00 pm
Network for Campus Representatives (NCR) Meeting
The Society of Pediatric Psychology's Network of Campus Representatives (NCR) Program is hosting an informal event for all current NCRs. At this meeting, co-chairs Melissa Engel and Mycah Ayala will provide important updates to the NCR Program, followed by Q&A and networking among NCRs to provide additional support and collaboration in creating events to increase awareness of pediatric psychology.
5:30 pm – 6:30 pm
Welcome Reception
(refreshments and light snacks)
Poster Session 1: Topics: Complementary and Integrative Medicine, Consultation-Liaison, Diabetes, Diversity, Medical Traumatic Stress, Obesity, Quality Improvement, Rehabilitation Medicine, and Solid Organ Transplant
On-Site Service & Outreach Activity - available at all poster sessions!
Lend a helping hand during the poster sessions by assembling to-go coffee kits for local families served by the Society of St. Vincent de Paul. Learn more about the Society of St. Vincent de Paul here: https://www.stvincentdepaul.net/. Contact: Desireé Williford, PhD, MPH (desiree.williford@cchmc.org)
7:00 pm – 8:00 pm
Student Social
We welcome trainees from all levels to join us for a team scavenger hunt in the hotel at 7pm. Winning team will receive a gift card! Following the Student Advisory Board-sponsored event, we will walk to a local bar for an informal gathering. A group will leave from the hotel lobby at 8:00 pm. Dress is casual.
Contact: Nicole Ruppe, M.S. (nruppe@okstate.edu), on behalf of the SPP Student Advisory Board
7:00 am
Registration and Check-In
7 am – 8 am
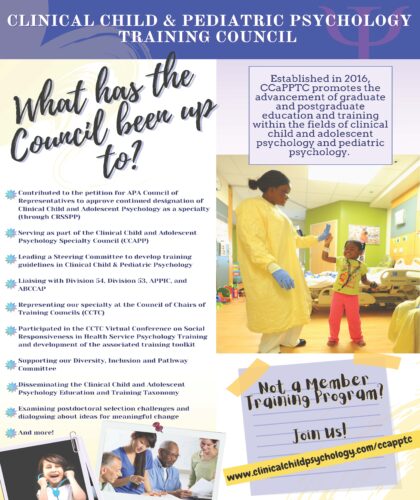
CCaPPTC Meeting
Established in 2016, the Clinical Child and Pediatric Psychology Training Council (CCaPPTC) promotes the advancement of graduate and postgraduate education and training in clinical child/adolescent and pediatric psychology. Members include doctoral, doctoral internship, and postdoctoral programs involved in the education and training of psychologists who work with children and families. All interested parties are welcome to join the meeting; Discussion will include: recent Council activities and current issues in training, updates about the activities of the Steering Committee for Training Guidelines, challenges related to postdoctoral selection and more.
8 am – 9 am
Breakfast
Poster Session 2: Topics: Advocacy, Allergic Diseases, Cardiology, Clinical Trials, Gastroenterology, Hematology/Oncology, Intervention Development, and Primary Care
On-Site Service & Outreach Activity - available at all poster sessions!
Lend a helping hand during the poster sessions by assembling to-go coffee kits for local families served by the Society of St. Vincent de Paul. Learn more about the Society of St. Vincent de Paul here: https://www.stvincentdepaul.net/. Contact: Desireé Williford, PhD, MPH (desiree.williford@cchmc.org)
Mid/Late Career Networking Event
Ready, Set, Network! Join us for a networking event for mid/late career professionals and invited speakers.
Chair: Natoshia Cunningham, PhD, on behalf of the SPPAC 2022 Scientific Program Committee
9 am – 11:15 am
Welcome Address
Awards
Plenary Address - Amplifying the Voice of Racial/Ethnic Minoritized Youth: Photo Stories & LEAP Projects
Margarita Alegría, PhD, Chief, Disparities Research Unit, Department of Medicine & the Mongan Institute, Massachusetts General Hospital; Harry G. Lehnert, Jr. and Lucille F. Cyr Endowed Chair, Mass General Research Institute, Massachusetts General Hospital; Professor, Departments of Medicine & Psychiatry, Harvard Medical School
Dr. Alegria will examine approaches to improve youth wellbeing and reduce inequality. She will share findings from her work with diverse youth as part of the PhotoStories project aimed at understanding racial/ethnic minority youths’ community-based experiences and emotional well-being. This presentation will emphasize how incorporating youth identified needs and feedback was pivotal in shaping the team’s conceptualization of their central issue and how it informed the next phase of their project. Dr. Alegria will then pivot to the specific elements that comprise the project’s next phase, LEAP.
Learning Objectives:
- Identify two benefits of soliciting youth co-researcher perspectives to enhance youth health promotion science
- Explain how maintaining a focus on youth perspectives can function as tool in community-engaged research.
- Describe one potential strategy for how to incorporate the principles of identifying problems and co-creating solutions with youth in intervention development.
Learner Level: Beginner to Immediate
11:30 am – 1:30 pm
LUNCH ON YOUR OWN
11:30am – 12:30pm
Student Mentoring Event
Prior registration was required and is now closed. This event is for students and trainees to meet and network with leaders in the field of pediatric psychology. Small groups of trainees are matched to a mentor with similar clinical/research/professional interests. This event is sponsored by Nemours Children’s Health. Food and drinks will be provided to registered attendees.
Contact: Clarissa Shields, M.A. (cshiel11@kent.edu), on behalf of the SPP Student Advisory Board
12:30 pm – 1:30 pm
ABCCAP INFORMATIONAL MEETING (CE)
Wendy Ward and Marsheena Murray
An Introduction to Board Certification through ABCCAP.
Learning Objectives:
Based on the content of the workshop attendees will be able to:
- Explain Foundational versus Functional Competencies
- Describe at least 3 benefits from being ABPP Board Certified
- Summarize the 3 stages in the board certification application process
1:30 pm – 2:30 pm
Plenary Address - Moving the Needle: Mentorship, Sponsorship and Allyship
During times of crisis, your network becomes even more vital. Successful leaders learn to build a network of mentors, sponsors and allies who will provide support, feedback, stability, and opportunities. This is particularly important for women and underrepresented minorities in medicine. Allyship in particular is critically important to changing culture and to support a diverse faculty.
Learning Objectives:
- Discuss the importance of leadership in times of crisis
- Articulate the necessity of mentorship and sponsorship to support leadership structures
- Utilize allyship to fight injustice
Learner Level: Introductory to Advanced
2:45 pm – 4:00 pm
Professional Development Breakouts
Advocacy for Pediatric Psychologists: Special considerations for Middle Eastern/North African Populations
Nicole Fleischer PsyD - St Christopher's Hospital for Children
Layli Khaghani PsyD - Private Practice
Saba Ahmadi MA - Alliant International University
Being Intentional When Addressing Diversity, Equity, and Inclusion in Pediatric Chronic Pain
Ethan Benore PhD - Cleveland Clinic
Elysia Soria MA - Cleveland Clinic
Jennifer Ramasami PhD - Cleveland Clinic
Empowering the Future Advocates and Leaders of Pediatric Psychology: Implications of Current Pandemics on Training and Beyond
Jeannette Iskander PhD - Akron Children's Hospital
Megan Schaefer PhD - Nationwide Children's Hospital
Idia Thurston PhD - Texas A & M
University Sharon Berry PhD - Children's Minnesota
Inclusion of Parents and Caregivers in Program Development and Quality Improvement Projects in Pediatric Medical Settings
Kendra Parris PhD - St. Jude Children's Research Hospital
Christina Salley PhD - Hassenfeld Children's Hospital at NYU Langone
Rachel Moore PhD - University of Missouri- Kansas City School of Medicine & Children's Mercy Hospital
The Roles of Pediatric Psychologists in Sustaining and Scaling Primary Care Integrated Behavioral Health Services
Kathryn Margolis PhD - UCSF
Melissa Buchholz PsyD - University of Colorado
Dominique Charlot-Swilley PhD - Georgetown University
Rahil Briggs PsyD - Zero to Three/Albert Einstein College of Medicine
Ayelet Talmi PhD - University of Colorado
4:00 pm – 4:30 pm
Break - Sponsored by American Board of Clinical Child Adolescent Psychology, a member board of the American Board of Professional Psychology
4:45 pm – 6:00 pm
Scientific Symposia Breakouts
Defining Successful Outcomes and Trade-offs (DSOT) for Clinical Management in Differences of Sex Development: A Mixed-Methods Approach to Inform Curriculum Development
Kristina Suorsa-Johnson PhD - University of Michigan
Erica Weidler MEd – Accord Alliance & Phoenix Children’s Hospital
Meilan Rutter MD - Cincinnati Children’s Hospital Medical Center & University of Cincinnati College of Medicine
David Sandberg PhD - University of Michigan
Top Rated Paper Abstracts: Disparities in Behavioral Health Referrals and Treatment
Chair: Thomaseo Burton, PhD, on behalf of the SPPAC 2022 Scientific Program Committee
Disparities in Children's Procedural Anxiety in the Emergency Department
Sarah Martin PhD - University of California Irvine School of Medicine
Theodore Heyming MD - Children's Hospital of Orange County
Michelle Fortier PhD - University of California Irvine
Brooke Valdez BS - Children's Hospital of Orange County
Zeev Kain MD MBA - University of California Irvine School of Medicine
Enhancing Interdisciplinary Collaboration Between Pediatric Primary Care and Schools: Primary Care Providers' Special Education Discussions with Families of Children with Autism
Mycah Ayala BS - University of Houston
My-Linh Luu MEd - University of Houston
Anna Laakman MEd - University of Houston
Sarah Mire PhD - University of Houston
Robin Kochel PhD - Baylor College of Medicine
Milena Keller-Margulis PhD - University of Houston
Weihua Fan PhD - University of Houston
Experiences of Caregivers of Children with Food Allergy during the COVID-19 Pandemic
Caroline Roberts MS - Oklahoma State University
Taylor Morgan MS - Oklahoma State University
Shahan Stutes MD - Oklahoma Allergy & Asthma Clinic
Dean Atkinson MD - Oklahoma Allergy & Asthma Clinic
Karen Gregory DNP APRN - Oklahoma Allergy & Asthma Clinic
Carrick Carter PsyD - University of Oklahoma Health Sciences Center
Larry Mullins PhD - Oklahoma State University
Alayna Tackett PhD - University of Southern California Keck School of Medicine
Physician Referral to Children’s Mental Health Services: A Cross-Cultural Examination of Contributing Factors
Ari Romano-Verthelyi MS - University of Connecticut
Interactive Digital Health Interventions During the COVID-19 Pandemic: Program Development, Patient Experiences, and Lessons Learned in Three Pediatric Populations
Corinne T. Evans BS - University of Alabama at Birmingham
Christina E. Holbein PhD - Children's Hospital of Philadelphia
Melissa L. Engel MA - Emory University
Rachelle R. Ramsey PhD - Cincinnati Children's Hospital Medical Center
The Society of Pediatric Psychology’s Anti Racism Grant Mechanism Recipients Symposium
Melissa Santos PhD - CT Children's
Virtual Intervention Feasibility and Recruitment/Retention Successes and Challenges in Pediatric Oncology during the COVID-19 Pandemic
Melissa Faith PhD ABPP - Johns Hopkins All Children's Hospital Johns Hopkins School of Medicine
Dianna Boone PhD - Johns Hopkins All Children's Hospital
Lamia Barakat PhD - Children's Hospital of Philadelphia
Kimberly Canter PhD - Nemours Children's Health System
Sarah Sobalvarro, Ph.D.- Johns Hopkins All Children’s Hospital, Johns Hopkins School of Medicine
6:30 pm – 7:30 pm
Internships and Fellowships on Parade
Dinner on your own
7:30 am
Registration and Check-In
8 am – 9 am
Breakfast
Poster Session 3 - Adolescent & Young Adult, Differences of Sex Development, Digital Health, Gender Health, Measure Development, Pain, Parents, and Patient & Family Voices
On-Site Service & Outreach Activity - available at all poster sessions!
Lend a helping hand during the poster sessions by assembling to-go coffee kits for local families served by the Society of St. Vincent de Paul. Learn more about the Society of St. Vincent de Paul here: https://www.stvincentdepaul.net/. Contact: Desireé Williford, PhD, MPH (desiree.williford@cchmc.org)
Early Career Networking Event:
Chair: Linda Herbert, PhD, on behalf of the SPPAC 2022 Scientific Program Committee
9 am – 10 am
Plenary Address - The Fierce Urgency of Now: Pediatric Psychologists as Policy Advocates
Learning Objectives:
- Describe accelerators and barriers to integrating advocacy and social justice into your professional identities
- Identify methods to effectively communicate psychological science to policy makers
- Discuss strategies to leverage research and clinical expertise to influence policy.
Learner Level: Intermediate
10:15 am – 11:30 am
Scientific Symposia Breakouts
Top Rated Paper Abstracts: Access to Behavioral and Mental Health Assessment & Treatment
Chair: Chad Jensen, PhD, on behalf of the SPPAC 2022 Scientific Program Committee
Developing a Summer Camp to Expose Youth in Underserved Areas to Psychology
Danielle Haggerty PhD - University of Michigan Michigan Medicine Division of Pediatric Psychology
Richard Birnbaum PhD - University of Michigan Michigan Medicine Division of Pediatric Psychology
Elizaveta Bourchtein PhD - University of Michigan Michigan Medicine Division of Pediatric Psychology
Sharnita D. Harris PhD - University of Michigan Michigan Medicine Division of Pediatric Psychology
Examining How California’s New Family Therapy Benefit Promotes Equitable Access to Preventative Behavioral Health Services in Primary Care: A HealthySteps Billing Study
Moorea Blythe PsyD - University of California San Francisco
Janelle Bercun LCSW - University of California San Francisco
Kathryn Hallinan LMFT - University of California San Francisco
Kathryn Margolis PhD - University of California San Francisco
Persons with Bleeding Disorders Identifying as Biological Females: Sugar, Spice, and Increased Risk of Psychosocial Concerns
Emily Wheat PhD - University of Colorado School of Medicine
Rich Shearer BA - University of Colorado Anschutz Medical Campus
Timothy Smith BA - University of Colorado Anschutz Medical Campus
Dianne Thornhill PhD - University of Colorado Anschutz Medical Campus
Kristi Norton BA - University of Colorado Anschutz Medical Campus
Julie Smith BA - University of Colorado Anschutz Medical Campus
System Changes in Pediatrics at Rush University Medical Center: Increasing Access to Behavioral Healthcare for West Side Youth
Emily Wolodiger PhD - Rush University Medical Center
Christina Iyengar MPH DrPH - Rush University Medical Center
Lashawnda Thornton MSW - Rush University Medical Center
Diamond Phillips BS - Rush University Medical Center
Allison Wainer PhD - Rush University Medical Center
Emerging Research in Gender Affirming Care for Transgender and Non-binary Youth
Jonathan Poquiz PhD - Johns Hopkins All Children's Hospital
Diane Chen - Ann & Robert H. Lurie children's Hospital of Chicago
Haley Hedrick, MS, MA - George Fox University
Discussant: Terry Stancin, PhD, ABPP, Case Western Reserve University School of Medicine
Innovative Approaches for Delivering Behavioral Pain Management Interventions in Pediatric Sickle Cell Disease and Cancer
Nicole Alberts PhD - Concordia University
Megan Connolly PhD - Children's National Hospital
Julia Johnston MA - University of South Carolina
Lindsay Jibb RN PhD CPHON - University of Toronto; Hospital for Sick Children
Supporting Patients, Parents, and Providers: Resource Development within Pediatric Differences of Sex Development
Kristina Suorsa-Johnson PhD - University of Michigan
Erica Weidler MEd – Accord Alliance & Phoenix Children’s Hospital
Danielle Moyer PhD - Oregon Health & Science University
Amy Tishelman PhD - Boston College
Project ECHO - Common to Complex: The Role of Pediatric Psychologists as Leaders, Collaborative Consultants and Educators for Primary Care Providers and Community-Based Mental Health Professionals
Melissa Young PsyD - Cincinnati Children's Hospital Medical Center
Jillian Austin PhD - Cincinnati Children's Hospital Medical Center
F. Lynne Merk PhD - Cincinnati Children's Hospital Medical Center
Jessica McClure PsyD - Cincinnati Children's Hospital Medical Center
11:30 am – 12:30 pm
Poster Session 4: Adherence, COVID-19, Craniofacial, Epilepsy, Nephrology, Sleep, Sports Medicine, Other, Late Breaking Posters
Sponsored by Cincinnati Children's Hospital Medical CenterOn-Site Service & Outreach Activity - available at all poster sessions!
Lend a helping hand during the poster sessions by assembling to-go coffee kits for local families served by the Society of St. Vincent de Paul. Learn more about the Society of St. Vincent de Paul here: https://www.stvincentdepaul.net/. Contact: Desireé Williford, PhD, MPH (desiree.williford@cchmc.org)
LUNCH
(boxed lunches available to attendees)
1 pm – 2:15 pm
Professional Development Breakouts
Ethical Implications of the Pandemic: Impact on Clinical Care, Program Development, and Training
Kate Eshleman PsyD - Cleveland Clinic Children’s
Dara Steinberg PhD - Columbia University Medical Center
Marissa Feldman PhD - Johns Hopkins All Children’s Hospital
Jami Gross -Toalson PhD - Children’s Mercy
Moving From Mastery to Accountability: Reflections on Cultural Humility in Training and Supervision
Colleen Cullinan PhD - Nemours Children's Health
Roger Harrison PhD - Nemours Children's Health
Marilyn Sampilo PhD MPH - Cleveland Clinic Children's
Avante Smack PhD - Children's National
Nikita Rodrigues PhD - Children's National
Pediatric Psychologists as Leaders Beyond the Hospital Walls: Community Access, Learning Health Networks, and Legislative Advocacy
Melissa Cousino PhD - University of Michigan C.S. Mott Children's Hospital
Lisa Ramirez PhD - MetroHealth System; Case Western School of Medicine
Meghan Walls PsyD - Nemours Health
Melissa McQueen Parent - Transplant Families
Sex, Drugs, and Rock and Roll: Screening, Assessment and Intervention of High-Risk Behaviors amongst Adolescents and Young Adults within the Integrated Primary Care Setting
Melissa Pielech PhD - Brown University
Melissa Young PsyD - Cincinnati Children's Hospital Medical Center
Christie Rizzo PhD - Northeastern University
Christopher Houck PhD - Brown University
The Role of the Pediatric Psychologist in Program Development: Practical Strategies for Turning Ideas into Action
Gillian Mayersohn PsyD - St. Louis Children's Hospital
Debra Lefkowitz PsyD - Children's Hospital of Philadelphia
Elizabeth Steinberg Christofferson PhD - Children's Hospital of Colorado
Kelli Triplett PhD ABPP - Children's Health Children's Medical Center Dallas
2:30 pm – 3:45 pm
Scientific Symposia Breakouts
Evidence-Based Practice in the Care of Transgender and Gender Diverse Youth: Exploring and Applying the World Professional Association for Transgender Health's Standards of Care
Julia Zeroth PhD - Nemours Children's Health
Amy Tishelman PhD - Boston College
Laura Edwards-Leeper PhD - Pacific University
Trisha Kumar MPH - OHSU-PSU School of Public Health
Neural Correlates and Biomarkers of Executive Function in Pediatric Chronic Illnesses
Kathryn King MA - University of Alabama at Birmingham
Amy Hughes-Lansing PhD - University of Vermont
Avani Modi PhD - Cincinnati Children's Hospital Medical Center
Marissa Gowey PhD - University of Alabama at Birmingham
Kyle Hill BS - Nationwide Children's Hospital
The View from Above: Leveraging Values-Based Payment Models to Develop Innovative Partnerships, Tools, and Strategies to Improve Population-Level Behavioral Health
Katherine Junger PhD - Cincinnati Children's Hospital
Jessica McClure PsyD - Cincinnati Children's
Erin Gonzalez PhD - Seattle Children's
Roy Jedeikin MD - Phoenix Children's Hospital
Turning the "Why" Into Innovative Models of Care: Addressing Health Inequities in Comprehensive Sickle Cell Clinics
Shweta Ghosh PhD - UCSF Benioff Children's Hospital Oakland
Julia LaMotte PhD - RIley Children's Hospital
Jeffrey Karst PhD - Medical College of Wisconsin Children's Wisconsin
Steven Hardy PhD - Children's National Hospital
Working with Linguistically and Culturally Diverse Patients and Families across Settings: Considerations and Implications
Paulina Lim MS - University of Wisconsin - Milwaukee
Amy Olen PhD - University of Wisconsin - Milwaukee
Laura Bava PhD ABPP - Children's Hospital of Los Angeles
Gabriela Vega MS - Nemours Children’s Hospital Delaware
Kimberly Canter PhD - Nemours Children’s Hospital Delaware